What is Meningitis?
Meningitis is an acute inflammation of the protective membranes covering the brain and spinal cord, known collectively as the meninges. This inflammation can be caused by infection with viruses, bacteria, or other microorganisms, and less commonly by certain drugs. Meningitis can be life-threatening due to the inflammation’s proximity to the brain and spinal cord; therefore, it is classified as a medical emergency.
Definition and Overview
Meningitis is characterized by the swelling of the meninges and is most often triggered by an infection. The severity and treatment differ significantly between cases of viral and bacterial meningitis, with bacterial meningitis being particularly severe and requiring immediate antibiotic treatment.
Causes of Meningitis
- Viral Meningitis: The most common form, often less severe, can be caused by enteroviruses, herpes simplex virus, HIV, and others.
- Bacterial Meningitis: More severe and potentially life-threatening, caused by bacteria such as Neisseria meningitidis, Streptococcus pneumoniae, and Haemophilus influenzae type b.
- Fungal Meningitis: Less common, typically occurs in individuals with weakened immune systems, caused by fungi such as Cryptococcus.
Symptoms and Early Warning Signs
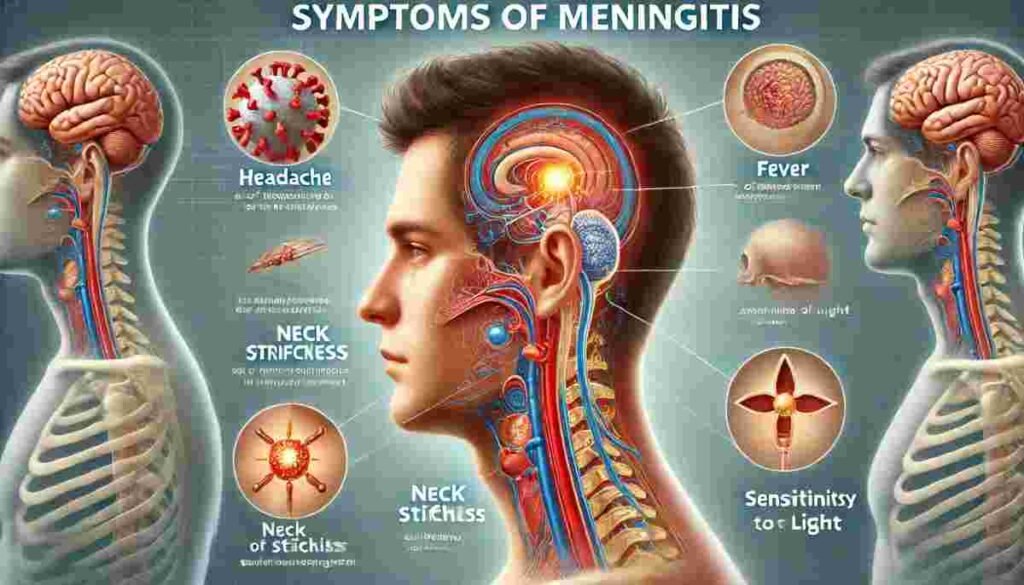
- Sudden high fever
- Severe headache
- Stiff neck
- Nausea or vomiting
- Confusion or difficulty concentrating
- Seizures
- Sleepiness or difficulty waking up
- Sensitivity to light
- No appetite or thirst
- Skin rash (in some cases of bacterial meningitis)
Diagnosis and Treatment of Meningitis
Diagnosing and treating meningitis promptly is critical due to the disease’s rapid progression and potential for severe complications. Understanding the diagnostic methods and treatment options can help in managing the condition effectively and minimizing long-term consequences.
Diagnosis of Meningitis
Meningitis diagnosis typically involves a combination of clinical evaluation and diagnostic tests. Here’s how it is generally approached:
- Clinical Evaluation: The first step often includes a detailed review of symptoms and medical history. Common symptoms of meningitis include severe headache, fever, neck stiffness, sensitivity to light, confusion, and in severe cases, seizures.
- Lumbar Puncture (Spinal Tap): This is the definitive test for diagnosing meningitis. It involves collecting a sample of cerebrospinal fluid (CSF) from the spinal canal through a needle. The fluid is then analyzed for signs of infection, such as increased white blood cells, proteins, and decreased glucose levels.
- Blood Tests: Blood cultures are done to identify bacteria that might have spread from another part of the body to the brain.
- Imaging Tests: CT or MRI scans of the head may be performed to rule out other conditions like brain abscesses or tumors that could cause similar symptoms.
- Other Tests: Depending on the suspected cause, additional tests like viral cultures, PCR testing for pathogens, and antigen tests may be used.
Treatment of Meningitis
Treatment depends on whether meningitis is viral, bacterial, or fungal:
Bacterial Meningitis:
- Antibiotics: High doses of intravenous antibiotics are administered as soon as bacterial meningitis is suspected, even before the diagnosis is confirmed. The type of antibiotic used depends on the age of the patient and the suspected bacterial strain.
- Corticosteroids: These can be used to reduce inflammation and prevent complications, such as swelling of the brain and seizures.
- Supportive Care: This includes fluids to prevent dehydration, oxygen for breathing difficulties, and antipyretics for fever.
Viral Meningitis:
- Supportive Care: Most cases of viral meningitis are milder and resolve without specific treatment. Supportive care might include rest, hydration, and over-the-counter pain relievers to help relieve symptoms.
- Antiviral Medications: These are occasionally used for certain types of viral infections, such as herpes meningitis.
Fungal Meningitis:
- Antifungal Medications: These are necessary for treating fungal meningitis and usually need to be taken for an extended period.
Adjunctive Therapy:
- Monitoring: Frequent monitoring of vital signs, hydration status, and neurological status is essential.
- Surgery: In cases where there are complications like brain swelling or abscess, surgical intervention may be necessary.
Preventive Measures
In addition to treatment, preventive measures are crucial. Vaccination is the most effective way to prevent meningitis caused by certain bacteria and viruses. Maintaining good hygiene, like washing hands and covering the mouth when coughing, can also help reduce the spread of infections that may lead to meningitis.
What is Meningitis Vaccine?
Types of Meningitis Vaccines
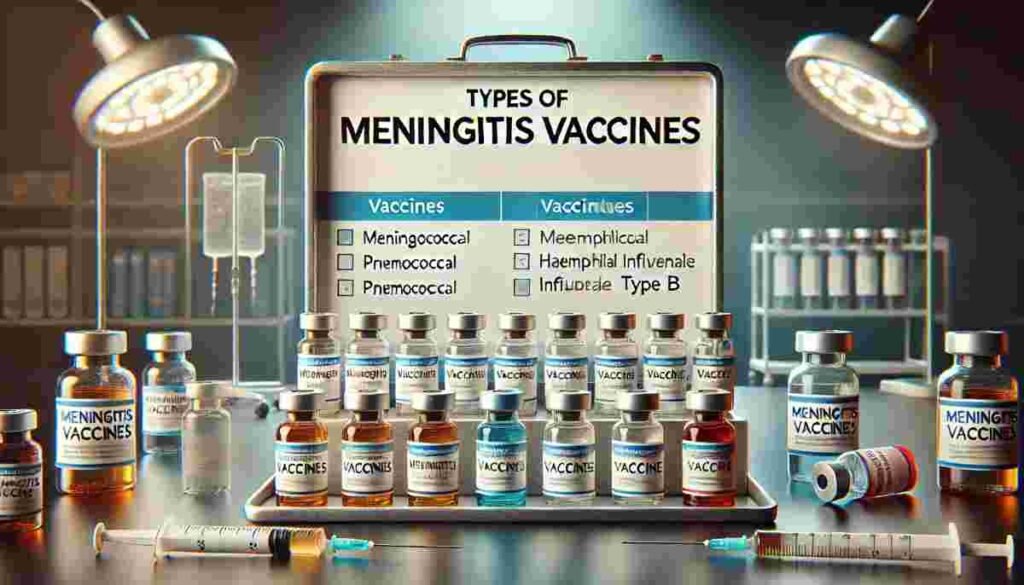
Vaccines are available for some types of bacterial and viral meningitis, providing effective prevention measures.
Bacterial Meningitis Vaccines
- Meningococcal Vaccines: Protect against most types of Neisseria meningitidis, available in conjugate and polysaccharide forms.
- Pneumococcal Vaccines: Effective against several types of Streptococcus pneumoniae.
- Hib Vaccine: Prevents Haemophilus influenzae type b meningitis.
Viral Meningitis Vaccines
While there are no specific vaccines for viral meningitis, vaccines for viruses that can cause meningitis, such as measles, mumps, and varicella (chickenpox), can prevent it.
Fungal Meningitis Prophylaxis
There are no vaccines for fungal meningitis; however, reducing exposure to environments where fungal pathogens thrive and managing pre-existing health conditions can help mitigate risk.
These detailed explanations provide a comprehensive understanding of meningitis, emphasizing the critical role of vaccines in preventing the bacterial forms of this disease and highlighting preventive measures for viral and fungal meningitis.
Key Bacterial Strains Covered by Vaccines
Meningococcal Vaccine
The meningococcal vaccine protects against Neisseria meningitidis, which causes meningococcal meningitis. This bacterium can lead to severe brain damage and is fatal in 50% of cases if untreated. There are several serogroups of N. meningitidis, with A, B, C, W, and Y being the most common in infections. Vaccines such as MenACWY and MenB are designed to protect against these serogroups.
Pneumococcal Vaccine
Pneumococcal vaccines target Streptococcus pneumoniae, which can cause pneumococcal meningitis among other infections like pneumonia and sepsis. Two main types of vaccines are available: Pneumococcal Conjugate Vaccine (PCV13) for children and Pneumococcal Polysaccharide Vaccine (PPSV23) for adults and certain high-risk groups.
Hib Vaccine
The Haemophilus influenzae type b (Hib) vaccine prevents meningitis caused by Hib bacteria. This was once the leading cause of bacterial meningitis in children under five before the widespread use of the vaccine.
Who Needs the Meningitis Vaccine?
Infants and Children
Infants and children are particularly vulnerable to bacterial meningitis, making vaccinations critical for this age group. Routine immunization schedules typically include vaccines for Haemophilus influenzae type b (Hib), pneumococcus (PCV13), and meningococcus (MenACWY for older children), starting from as early as a few months old.
Adolescents and College Students
Adolescents and college students are at increased risk, particularly when entering environments such as college dormitories where close contact can promote the spread of bacteria. The meningococcal vaccine (MenACWY) is especially recommended for first-year college students living in dormitories.
Travelers and Military Personnel
Vaccinations are also advised for individuals traveling to or residing in countries where meningitis is common, as well as for military personnel who often live in close quarters. These settings increase the risk of contracting meningococcal disease.
Vaccine Schedule and Dosage
Recommended Age for Vaccination
The appropriate age for administering meningitis vaccines varies based on the type of vaccine. For instance:
- Hib Vaccine: The first dose is usually given at two months old.
- Pneumococcal Vaccine (PCV13): Administered at 2, 4, 6, and 12-15 months.
- Meningococcal Vaccine (MenACWY): First dose at 11-12 years with a booster at 16 years old.
- MenB Vaccine: Recommended for teens and young adults, although the schedule can vary based on the brand and risk factors.
Booster Doses
Booster doses are essential to extend the vaccine’s protection. For example, the MenACWY vaccine requires a booster shot at age 16 to ensure continued protection throughout adolescence and into adulthood.
Catch-up Vaccinations
Catch-up vaccinations are vital for those who missed initial doses or boosters. They ensure individuals are protected against meningitis, especially during outbreaks or in high-risk settings.
Benefits of Vaccination
Vaccination stands as one of the most significant medical breakthroughs, offering protection against various infectious diseases, including meningitis. Here’s a closer look at the critical benefits of meningitis vaccination:
Prevention of Disease Spread
Vaccines are designed to protect not only the individuals receiving them but also the broader community by preventing the spread of infectious agents. Meningitis, particularly the bacterial type, can be highly contagious. It is spread through respiratory and throat secretions (e.g., saliva, kissing, coughing).
Vaccinating a significant portion of the population helps reduce the number of potential carriers and the spread of the disease, thus protecting those who are unvaccinated or those who cannot receive the vaccine due to medical conditions.
Reduction in Long-Term Complications
Meningitis can cause severe health complications if not treated promptly, including hearing loss, brain damage, learning disabilities, and even death. The vaccination significantly reduces the risk of these severe outcomes by preventing the disease’s occurrence in the first place.
For many, particularly children and the elderly who are at higher risk, this can mean a substantial difference in life quality, reducing the likelihood of permanent disabilities that result from the disease.
Community Immunity Benefits
Community immunity, or herd immunity, occurs when a sufficient portion of the population is immunized against a contagious disease, making its spread from person to person unlikely. This form of protection is crucial for those who cannot be vaccinated, such as newborns, those with chronic illnesses, or people with weakened immune systems.
By vaccinating the majority, the community as a whole is less likely to face outbreaks, which can be particularly devastating in closed or highly populated environments like schools, colleges, and nursing homes.
Safety and Side Effects
Common Side Effects
The most frequent side effects of meningitis vaccines are mild and include:
- Redness or pain at the injection site
- Mild fever
- Fatigue
- Irritability in children
These symptoms typically resolve without medical intervention within a few days.
Rare Complications
While very rare, severe allergic reactions can occur, such as anaphylaxis. Immediate medical attention is crucial if symptoms like difficulty breathing, swelling of the face or throat, or a severe rash develop.
Managing Side Effects
Most side effects can be managed at home with simple remedies such as:
- Applying a cool compress to reduce soreness at the injection site
- Using over-the-counter pain relievers like acetaminophen or ibuprofen to alleviate pain and fever
Future Directions in Meningitis Prevention
Advancements in prevention strategies are crucial for reducing the global burden of meningitis. This involves ongoing research and development, innovative vaccine technologies, and collaborative efforts in global health strategies. Here’s an in-depth look at these future directions:
Research and Development
Research and development in meningitis prevention continue to evolve, focusing on improving current vaccines and developing new ones. Key areas include:
- Broader Spectrum Vaccines: Current research is focused on developing vaccines that cover a wider range of meningitis-causing bacteria and viruses. This includes efforts to create a universal pneumococcal vaccine that can provide coverage against multiple strains of the bacteria.
- Improved Vaccine Delivery Systems: Researchers are exploring more efficient vaccine delivery systems, such as nasal sprays or patches, which could improve immunization rates by providing easier and less invasive administration methods.
- Enhanced Diagnostic Tools: Developing faster and more accurate diagnostic tools can lead to quicker treatment and better outcomes. Point-of-care tests that can be administered in remote or resource-limited settings are a significant focus.
New Vaccine Technologies
Innovation in vaccine technology is pivotal for advancing meningitis prevention. Emerging technologies include:
- mRNA Vaccines: Inspired by the success of mRNA COVID-19 vaccines, researchers are investigating the use of mRNA technology for meningitis vaccines. This method allows for rapid development and adaptation in response to emerging strains.
- Conjugate Vaccines: These vaccines, which link antigens to a protein to improve the immune response, are being enhanced to include multiple antigens from different meningitis pathogens, offering broader protection.
- Adjuvant Improvements: Adjuvants are substances added to vaccines to enhance the immune response. Research is ongoing to discover new adjuvants that can make vaccines more effective, especially among populations with weaker immune systems, like the elderly.
Collaborative Global Health Strategies
Collaborative efforts are essential for the widespread implementation of meningitis prevention strategies, especially in low-resource areas:
- Global Vaccination Programs: Organizations like the World Health Organization (WHO) and GAVI, the Vaccine Alliance, are expanding their efforts to include meningitis vaccines in national immunization programs worldwide, particularly in regions with high incidence rates.
- Integration with Other Health Services: Integrating meningitis vaccination with other routine health services can improve coverage. For instance, offering meningitis vaccines alongside maternal and child health services ensures broader immunization coverage.
- Public Health Campaigns and Education: Increasing public awareness about meningitis and the importance of vaccination through global health campaigns can drive higher vaccination rates and encourage early treatment seeking.
- Data Sharing and Surveillance: Enhancing global surveillance systems and sharing data between countries help monitor and respond to meningitis outbreaks more effectively. This global network is crucial for identifying hotspots and deploying resources accordingly.
Key Takeaways
- Critical Protection: The meningitis vaccine is essential for protecting individuals from a potentially deadly infection that can cause severe brain damage and other long-term disabilities.
- Community Health: Vaccination not only protects the individual but also aids in creating herd immunity, which is crucial in preventing outbreaks.
- Safety and Efficacy: Meningitis vaccines have a strong safety record and are highly effective in preventing the disease, significantly reducing the incidence of meningitis globally.
- Inclusive Recommendations: It’s recommended for infants, adolescents, and people with certain medical conditions or those traveling to countries where meningitis is common, highlighting the importance of widespread immunization programs.
FAQs
Q1: Can the meningitis vaccine prevent all types of meningitis?
A: No, meningitis vaccines specifically target bacteria and viruses that commonly cause the disease. They are highly effective against certain types, like bacterial meningitis caused by Neisseria meningitidis, Streptococcus pneumoniae, and Haemophilus influenzae type b. However, they do not prevent viral meningitis caused by non-vaccine viruses or fungal meningitis.
Q2: What are the five symptoms of meningitis?
A: The five key symptoms of meningitis include a sudden high fever, severe headache, stiff neck, nausea or vomiting, and increased sensitivity to light. These symptoms can develop rapidly and require immediate medical attention to prevent serious complications and improve outcomes.
Q3: Is the meningitis vaccine required for school entry?
A: Requirements vary by region, but many areas require children to receive the meningitis vaccine before starting school, especially for entry into residential settings like boarding schools and colleges. It’s essential to consult local health regulations to understand the specific vaccine requirements.
Q4: Are there any individuals who should not receive the meningitis vaccine?
A: Individuals with severe allergies to any component of the vaccine should not receive it. Those with moderate or severe acute illnesses should wait until recovery. The appropriateness of vaccination for people with other specific medical conditions should be discussed with a healthcare provider.
Q5: What are the signs that someone may be having a severe reaction to the meningitis vaccine?
A: Signs of a severe reaction include difficulty breathing, swelling of the face or throat, hives, a fast heartbeat, dizziness, and weakness. These symptoms can occur within a few hours of vaccination and require immediate medical attention.
Conclusion
Meningitis remains a critical public health concern due to its potential severity and rapid progression. Vaccination plays a vital role in controlling and preventing various forms of meningitis, particularly those caused by bacteria such as Neisseria meningitidis, Streptococcus pneumoniae, and Haemophilus influenzae type b. Through routine immunization, booster doses, and adherence to recommended schedules, individuals can significantly reduce their risk of contracting this potentially fatal disease.
The safety profile of meningitis vaccines is favorable, with common side effects being mild and manageable. While severe reactions are rare, awareness of these possible reactions ensures that individuals can seek prompt medical care, further ensuring the safety of the vaccination process.
