What is an Inhaler?
Definition
An inhaler is a handheld medical device used to deliver medication directly into the lungs, making it essential for managing respiratory conditions such as asthma, chronic obstructive pulmonary disease (COPD), and allergies. Inhalers come in various forms, including metered-dose inhalers (MDI), dry powder inhalers (DPI), and soft mist inhalers (SMI). These devices are compact and easy to carry, allowing individuals to have quick access to medication whenever needed.
Importance
Inhalers are vital for people with chronic respiratory diseases, as they provide immediate relief from symptoms such as shortness of breath, wheezing, and coughing. These devices not only help manage acute asthma attacks or COPD flare-ups but also play a critical role in long-term maintenance by delivering corticosteroids or bronchodilators directly to the lungs. This allows for better control of symptoms, fewer emergency situations, and an improved quality of life.
For many patients, inhalers act as a lifeline. The portability of inhalers ensures that users can carry them wherever they go, ensuring timely treatment in case of unexpected breathing difficulties.
How Inhalers Work
Inhalers work by converting medication into a fine mist or powder that can be inhaled deeply into the lungs. Once inhaled, the medication targets the airways directly, leading to quick relief of symptoms.
Different inhalers have distinct mechanisms:
- Metered-dose inhalers (MDIs) release a measured amount of medication using a propellant.
- Dry powder inhalers (DPIs) require the user to take a quick, deep breath to draw the powdered medication into the lungs.
- Soft mist inhalers (SMIs) create a fine mist of medication, which can be inhaled more gently.
By delivering medication directly to the lungs, inhalers allow for faster action compared to oral or injected medications, making them incredibly effective for both emergency and long-term respiratory care.
Types of Inhalers

When it comes to managing respiratory conditions, different types of inhalers are designed to deliver medication effectively based on a patient’s specific needs. Below, we explore the three main types of inhalers: Metered-Dose Inhalers (MDIs), Dry Powder Inhalers (DPIs), and Soft Mist Inhalers (SMIs), each offering unique benefits and features.
Metered-Dose Inhalers (MDI)
Metered-Dose Inhalers, or MDIs, are one of the most common types of inhalers. They work by delivering a specific amount of medication with each press, usually using a chemical propellant. MDIs are widely used for conditions like asthma and COPD, providing quick relief from symptoms by delivering bronchodilators or corticosteroids directly into the lungs. These inhalers are portable and easy to use, but proper technique is essential for effective medication delivery. Many people use a spacer with MDIs, which helps ensure the medication reaches the lungs instead of being deposited in the mouth or throat.
Dry Powder Inhalers (DPI)
Dry Powder Inhalers (DPIs) offer an alternative for people who may have difficulty using MDIs. Instead of a propellant, DPIs rely on the user’s inhalation to release the medication in the form of a dry powder. This type of inhaler is breath-activated, making it easier for those who struggle with the coordination required for MDIs. DPIs are often prescribed for long-term management of chronic respiratory conditions. However, they require the user to have a strong enough inhalation effort to effectively pull the medication into the lungs, which may be challenging during a severe asthma attack.
Soft Mist Inhalers (SMI)
Soft Mist Inhalers (SMIs) are a newer type of inhaler that produce a slow-moving, fine mist of medication without the need for a propellant. The slow release of medication makes SMIs easier to inhale, allowing more of the medicine to reach the lungs. These inhalers are especially beneficial for people with limited lung capacity or those who struggle to use MDIs or DPIs. The soft mist helps improve the delivery of medication, reducing the need for a spacer, though spacers can still be used for added convenience. SMIs are typically used for conditions requiring long-term treatment, like COPD and asthma.
How to Use an Inhaler Correctly

Using an inhaler correctly is essential to ensure you receive the full dose of medication and manage your respiratory condition effectively. Many people may not be aware that improper inhaler technique can lead to reduced medication delivery and, subsequently, less control over symptoms. Below is a step-by-step guide to using an inhaler, common mistakes to avoid, and the importance of using a spacer for optimal results.
Step-by-Step Guide
- Shake the Inhaler: If you are using a metered-dose inhaler (MDI), shake it well before use. This helps ensure the medication is properly mixed and ready for delivery.
- Remove the Cap: Take off the inhaler cap and inspect the mouthpiece to make sure it’s clean and free of debris.
- Breathe Out Completely: Before inhaling the medication, breathe out fully. This step ensures that your lungs are ready to receive the medication.
- Position the Inhaler: Hold the inhaler upright with the mouthpiece at the bottom. Place the mouthpiece in your mouth, ensuring a good seal with your lips.
- Press the Inhaler and inhaler: As you begin to breathe in slowly, press down on the inhaler to release the medication. Keep on taking in profoundly and consistently.
- Hold Your Breath: Hold your breath for 5-10 seconds after inhaling the medication. This allows the medication to settle in your lungs.
- Exhale Slowly: After holding your breath, exhale slowly and calmly.
- Repeat if Necessary: If a second dose is required, wait about 30 seconds to a minute before repeating the process.
- Rinse Your Mouth (if using corticosteroids): If your inhaler contains a corticosteroid, rinse your mouth with water after use to prevent irritation and oral infections.
Common Mistakes
- Not Breathing In Properly: One of the most common mistakes people make is not coordinating their inhalation with the release of the medication. This can result in the medication being deposited in the mouth or throat instead of the lungs.
- Not Shaking the Inhaler: Failing to shake a metered-dose inhaler can lead to uneven doses of medication, meaning you might not get the full therapeutic effect.
- Inhaling Too Quickly: Rapid inhalation can cause the medication to hit the back of the throat instead of reaching the lungs. Inhalation should be slow and steady for maximum effectiveness.
- Skipping the Exhalation Step: Not fully exhaling before using the inhaler can leave less room in the lungs for the medication, reducing its effectiveness.
- Forgetting to Clean the Inhaler: A dirty inhaler can become clogged, preventing proper delivery of medication. Cleaning the inhaler regularly is vital for maintaining its efficiency.
Importance of a Spacer
A spacer is a tube that attaches to your inhaler, and it helps deliver the medication more effectively by allowing you to breathe in the medication at your own pace. Spacers are especially helpful for children, older adults, or anyone who struggles with coordinating inhalation with the release of the medication from the inhaler.
Here’s why a spacer can improve inhaler use:
- Increased Medication Delivery: Spacers help reduce the amount of medication that settles in the mouth and throat, directing more of the drug into the lungs where it’s needed.
- Reduced Side Effects: For inhalers that contain corticosteroids, using a spacer can help reduce side effects like oral thrush or hoarseness, as less medication is deposited in the mouth.
- Improved Ease of Use: Spacers eliminate the need to precisely time inhalation with the release of the medication, making it easier for those with limited lung function or coordination issues.
Incorporating a spacer into your inhaler routine can enhance medication effectiveness and reduce the likelihood of mistakes, making it a valuable tool in managing respiratory conditions like asthma and COPD.
Inhaler Medications

Inhalers deliver various types of medications to the lungs to manage respiratory conditions such as asthma and COPD. These medications work to either relieve symptoms quickly or control inflammation over the long term. Below are the main categories of inhaler medications, including bronchodilators, corticosteroids, and combination inhalers.
Bronchodilators
Bronchodilators are medications that relax the muscles around the airways, making it easier to breathe by opening the airways. These are commonly used to provide quick relief during an asthma attack or flare-up of COPD symptoms. Bronchodilators are divided into two categories: short-acting and long-acting.
- Short-acting bronchodilators provide rapid relief from symptoms and are typically used in emergencies to alleviate sudden breathing difficulties.
- Long-acting bronchodilators are used for maintaining long-term control of symptoms, especially in COPD patients.
Corticosteroids
Corticosteroids are anti-inflammatory medications that help reduce inflammation in the airways, making them effective for long-term control of asthma and COPD symptoms. They do not provide immediate relief but are essential for managing chronic respiratory conditions by preventing flare-ups.
- Inhaled corticosteroids are commonly used as a first-line treatment for persistent asthma.
- These medications reduce swelling in the airways, making it easier for patients to breathe over time.
Combination Inhalers
Combination inhalers contain both a bronchodilator and a corticosteroid, providing both quick relief and long-term control. These inhalers are often prescribed for people who need more than one type of medication to manage their condition.
- Combination inhalers help reduce the frequency of asthma attacks and improve overall lung function.
- They are typically used for moderate to severe asthma or COPD and provide the benefits of both bronchodilators and anti-inflammatory agents in one device.
Inhalers for Asthma
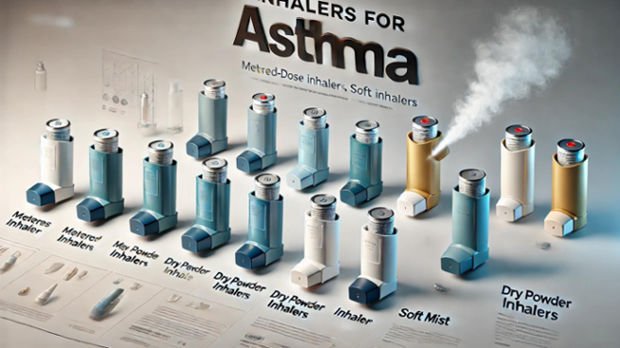
Asthma inhalers are divided into two main categories: quick-relief inhalers for immediate symptom relief and long-term control inhalers for ongoing management of asthma. Both types are essential for maintaining effective asthma control.
Quick-Relief Inhalers
Quick-relief inhalers, also known as rescue inhalers, provide fast-acting medication that works within minutes to relieve symptoms such as wheezing, coughing, and shortness of breath. These inhalers contain short-acting bronchodilators like albuterol, which help relax the muscles around the airways.
- When to use: During an asthma attack or when experiencing sudden difficulty breathing.
- Key Benefit: Quick symptom relief.
Long-Term Control Inhalers
Long-term control inhalers are used daily to prevent asthma symptoms and keep the condition under control. These inhalers usually contain corticosteroids, which help reduce inflammation in the airways over time. Unlike quick-relief inhalers, they do not provide immediate relief but are crucial for preventing asthma attacks.
- When to use: Every day, even when symptoms are not present, for ongoing management.
- Key Benefit: Prevents asthma flare-ups and controls chronic symptoms.
How to Choose the Right Inhaler
Choosing the right inhaler depends on several factors, including the severity of your condition, your symptoms, and how well you can use the inhaler. Here are a few ways to pursue the ideal decision:
- For quick relief: If you experience sudden symptoms or asthma attacks, a quick-relief inhaler with a short-acting bronchodilator like albuterol is essential.
- For long-term management: If you have persistent asthma, a long-term control inhaler with a corticosteroid or combination inhaler is necessary for daily use.
- Consult with your doctor: Your healthcare provider can assess your condition and prescribe the right inhaler based on your needs, including whether you need one or both types of inhalers.
Inhalers for COPD

Chronic Obstructive Pulmonary Disease (COPD) is a progressive respiratory condition that requires effective management to reduce symptoms and improve quality of life. Inhalers are one of the primary treatment options for COPD, delivering medications directly to the lungs to help open airways, reduce inflammation, and improve breathing. Below, we delve into the best inhalers for COPD management, the differences between inhalers for COPD and asthma, and the essential role that inhalers play in COPD treatment.
Best Inhalers for COPD Management
COPD treatment usually involves a combination of inhalers, each designed for different purposes. Probably the best kinds include:
- Bronchodilators: These inhalers help relax the muscles around the airways, making it easier to breathe. Short-acting bronchodilators like albuterol are used for quick relief, while long-acting bronchodilators like tiotropium (Spiriva) are used for ongoing management.
- Corticosteroids: Inhaled corticosteroids like budesonide or fluticasone help reduce inflammation in the lungs. These are usually prescribed for individuals with more severe COPD or frequent flare-ups.
- Combination Inhalers: These inhalers contain both a bronchodilator and a corticosteroid for dual action, offering long-term relief from symptoms and inflammation.
Differences Between COPD and Asthma Inhalers
While inhalers for both COPD and asthma may seem similar, they are often designed for different purposes and treatments.
- Duration of Action: COPD patients typically require long-acting bronchodilators for continuous symptom management, while asthma patients may use more short-acting inhalers for quick relief during attacks.
- Medication Combinations: COPD inhalers frequently combine bronchodilators and corticosteroids to reduce inflammation and improve lung function, whereas asthma inhalers might rely more on short-term bronchodilators and specific medications to prevent flare-ups.
- Symptom Management: Inhalers for asthma are often used in emergencies to alleviate sudden symptoms. On the other hand, COPD inhalers are more often used as part of a long-term treatment strategy to manage day-to-day breathing difficulties.
The Role of Inhalers in COPD Treatment
Inhalers are a cornerstone of COPD treatment, offering several benefits:
- Symptom Control: Inhalers help manage symptoms such as breathlessness, coughing, and wheezing by delivering medication directly to the lungs, which improves oxygen flow and overall lung function.
- Prevention of Flare-ups: By reducing inflammation and keeping airways open, inhalers help prevent exacerbations, or flare-ups, that could lead to hospitalization or worsening of the condition.
- Improved Quality of Life: With regular use, inhalers can significantly improve the quality of life for COPD patients by enabling better lung function and reducing the frequency of breathing difficulties.
Common Side Effects of Using an Inhaler
While inhalers are essential for managing conditions like asthma and COPD, they can also cause some side effects. It is important to be aware of both short-term and long-term effects to use inhalers safely and effectively. Below are some common side effects and advice on when to seek medical help.
Short-Term Side Effects
- Dry Mouth and Throat Irritation: One of the most common side effects of inhaler use, especially with corticosteroids, is dry mouth or a sore throat. This occurs because the medication can irritate the oral and throat tissues.
- Coughing or Hoarseness: Some people may experience coughing, hoarseness, or a slight burning sensation in their throat immediately after using their inhaler. These symptoms usually pass quickly and can be reduced by using a spacer or rinsing your mouth after use.
- Increased Heart Rate: Some inhalers, especially bronchodilators, can cause an increase in heart rate, leading to a sensation of palpitations or jitteriness. These effects are typically short-lived but should be monitored.
Long-Term Side Effects
- Oral Thrush: Inhalers that contain corticosteroids can lead to a yeast infection in the mouth called oral thrush. This can be minimized by rinsing your mouth with water after each use.
- Bone Density Loss: Long-term use of inhaled corticosteroids, particularly at high doses, can lead to reduced bone density, increasing the risk of osteoporosis. It is important to have regular bone density scans if you are on prolonged corticosteroid therapy.
- Suppression of Adrenal Glands: Chronic use of corticosteroids can sometimes suppress the adrenal glands, which play a key role in hormone production. This side effect is more likely with high doses or long-term use.
When to Contact a Doctor
It’s important to stay alert for any side effects that may indicate a more serious issue. You ought to contact your PCP assuming that you experience:
- Severe Difficulty Breathing: If using your inhaler does not relieve your breathing difficulties, or if you find that you need to use your quick-relief inhaler more frequently than prescribed, this could indicate a worsening of your condition.
- Allergic Reactions: Though rare, some people may experience an allergic reaction to the medication in their inhaler. Symptoms might include swelling of the lips, tongue, or throat, hives, or difficulty breathing. This requires immediate medical attention.
- Persistent Side Effects: If you notice that short-term side effects such as a fast heart rate, hoarseness, or dry mouth persist or worsen, it’s a good idea to consult with your doctor. They may need to adjust your medication or recommend a different type of inhaler.
Maintaining and Cleaning Your Inhaler
Proper maintenance and cleaning of your inhaler are crucial for ensuring it delivers the correct dose of medication and prevents blockages or contamination. A clean and well-maintained inhaler functions more efficiently, reducing the risk of infections or reduced efficacy over time. Here’s a detailed guide on how often to clean your inhaler, the steps involved, and the best storage practices.
How Often to Clean an Inhaler
Inhalers should be cleaned regularly to maintain their effectiveness. Generally, it is recommended to clean your inhaler once a week. Regular cleaning prevents the buildup of medication residue or dust, which can block the inhaler and affect the dosage delivered. If you notice a drop in the effectiveness of your inhaler or experience difficulty in pressing it, this may also indicate that it needs to be cleaned more frequently.
Steps to Cleaning an Inhaler
Cleaning an inhaler is a straightforward process, but it’s important to follow the correct steps to avoid damaging the device:
- Remove the medication canister: Start by separating the medication canister from the plastic mouthpiece. Be careful not to wash the canister itself, as water can damage it.
- Rinse the mouthpiece: Hold the plastic mouthpiece under warm running water for 30-60 seconds. This helps to remove any medication buildup, dust, or debris. Ensure that water flows through the small opening where the medication is released.
- Shake off excess water: After rinsing, shake off any excess water and allow the mouthpiece to air dry completely. It’s important to make sure the mouthpiece is completely dry before reassembling it, as moisture can interfere with the inhaler’s function.
- Wipe the canister: While the mouthpiece dries, use a clean, dry cloth to wipe the outside of the medication canister. Try not to lower the canister in water.
- Reassemble the inhaler: Once the mouthpiece is fully dry, reinsert the medication canister and ensure the inhaler is functioning correctly by giving it a test spray if recommended by your doctor.
Storage Tips for Inhalers
Proper storage of your inhaler is just as important as regular cleaning to maintain its functionality:
- Keep it in a dry place: Moisture can damage the inhaler, so it’s best to store it in a dry environment. Avoid storing your inhaler in a bathroom or other humid areas.
- Store at room temperature: Extreme temperatures can affect the medication’s efficacy. It’s important to store your inhaler at room temperature, avoiding both very hot and very cold environments. For instance, leaving it in a hot car or exposing it to freezing conditions can degrade the medication inside.
- Cap the mouthpiece: Always put the cap back on the mouthpiece after use. This prevents dust and dirt from getting inside and helps maintain hygiene.
- Check the expiration date: Ensure you’re aware of the expiration date on your inhaler. Using an expired inhaler may result in receiving less than the required dose of medication.
Inhaler Misuse and Misunderstandings
Although inhalers are essential tools for managing respiratory conditions like asthma and COPD, misuse is common, leading to ineffective treatment or even worsening symptoms. Understanding proper inhaler usage is critical for getting the full benefits of the medication. Below, we discuss common misuse scenarios, debunk myths, and emphasize the importance of following a prescription.
Overuse and Underuse
One of the most significant issues with inhaler use is finding the right balance between overuse and underuse. Overuse occurs when patients rely too heavily on quick-relief inhalers (like bronchodilators) for immediate symptom relief instead of following a long-term treatment plan. This can lead to medication tolerance, where the body becomes less responsive to the medication, requiring higher doses for the same effect. In severe cases, overuse can mask the worsening of the underlying condition, delaying essential medical treatment.
Myths About Inhalers
There are several misconceptions about inhaler use that can lead to improper management of respiratory conditions. One common myth is that inhalers are only needed during an asthma attack or flare-up. This belief can lead to patients neglecting their daily maintenance inhalers, which are crucial for preventing attacks and managing chronic inflammation. Another widespread misconception is that using an inhaler will result in dependence, meaning the body will stop being able to function without it. This is not true; inhalers are designed to manage the symptoms of asthma and COPD, not to create dependency. The medication delivered through an inhaler helps reduce inflammation and open airways, improving quality of life without the risk of dependence.
The Importance of Following a Prescription
The key to effective inhaler use is strictly following a healthcare provider’s prescription. Inhalers are not “one-size-fits-all” devices. Each prescription is tailored to the individual’s condition, symptoms, and overall health. Ignoring a prescribed treatment plan, either by using the inhaler too frequently or not enough, can lead to uncontrolled symptoms or worsened respiratory health.
FAQs About Inhaler
Q1. When should I use an inhaler?
A: You should use a quick-relief inhaler during an asthma attack or when experiencing sudden breathing difficulties. Maintenance inhalers should be used daily as prescribed to prevent attacks and manage long-term symptoms. Continuously heed your primary care physician’s guidance in regards to the recurrence of purpose.
Q2. How does an inhaler work?
A: Inhalers deliver medication directly into the lungs through aerosolized particles or powder. This medication helps to open the airways (bronchodilators) or reduce inflammation (corticosteroids), making it easier to breathe. The direct delivery to the lungs ensures fast and efficient relief of symptoms.
Q3. Does an inhaler have side effects?
A: Yes, inhalers can have side effects, such as dry mouth, throat irritation, and in some cases, an increased heart rate. Long-term use of corticosteroid inhalers may lead to more serious side effects, like oral thrush. It’s essential to use the inhaler correctly to minimize these effects.
Q4. What is the mechanism of action of the inhaler?
A: Inhalers work by delivering medication directly to the lungs. Bronchodilators relax the muscles around the airways, allowing them to open up, while corticosteroids reduce inflammation and swelling in the airways. This helps improve airflow and ease breathing.
Q5. What is the difference between a nebulizer and an inhaler?
A: An inhaler is portable and delivers a quick dose of medication with each use, while a nebulizer converts liquid medication into a mist that is inhaled over a longer period. Nebulizers are typically used for patients who have difficulty using inhalers, but they are less convenient for on-the-go use.
Conclusion
Inhalers are an indispensable tool for managing respiratory conditions like asthma and COPD, providing quick relief and long-term control of symptoms. With different types of inhalers available—metered-dose inhalers (MDI), dry powder inhalers (DPI), and soft mist inhalers (SMI)—patients have options to suit their specific needs. Correct usage, regular maintenance, and adherence to prescribed treatment plans are crucial for ensuring the effectiveness of inhalers.
While there may be some misconceptions and potential side effects, understanding how inhalers work and using them properly can significantly improve quality of life. Whether you’re a new or long-time user, staying informed and working closely with your healthcare provider is essential for optimal respiratory health.
